Do maxillofacial surgeon diagnose Oral Cancer & Tumour ?

Maxillofacial surgeons play a crucial role in the diagnosis and treatment of oral cancer and tumors. Here are some of the procedures and treatments they may perform:
1. Oral Cancer Screening: Maxillofacial surgeons are trained to detect early signs of oral cancer through thorough oral examinations, including inspecting the mouth, throat, and neck for any abnormalities or suspicious lesions.
2. Biopsy: If a suspicious area is found, a maxillofacial surgeon may perform a biopsy to collect tissue samples for laboratory analysis. This helps in confirming the presence of cancer cells and determining the type and stage of the cancer.
3. Tumor Removal: Maxillofacial surgeons are skilled in surgical techniques to remove cancerous tumors from the oral cavity, jaws, and surrounding structures. The extent of the surgery depends on the size, location, and stage of the tumor.
4. Reconstructive Surgery: After tumor removal, maxillofacial surgeons can perform reconstructive procedures to restore the appearance and functionality of the affected areas. This may involve grafting procedures, dental implants, and the use of advanced techniques like microvascular surgery.
5. Adjuvant Therapies: Maxillofacial surgeons work in collaboration with other healthcare professionals to develop comprehensive treatment plans. They may recommend adjuvant therapies such as radiation therapy or chemotherapy to target any remaining cancer cells and improve long-term outcomes.
6. Follow-up Care: Maxillofacial surgeons provide ongoing monitoring and follow-up care to ensure that the patient’s oral health is maintained and any potential recurrence or complications are detected early.
It’s important to consult with a maxillofacial surgeon or an oral and maxillofacial specialist if you suspect or have been diagnosed with oral cancer or tumors. They have the expertise and experience to provide accurate diagnosis, personalized treatment plans, and comprehensive care throughout the entire process.
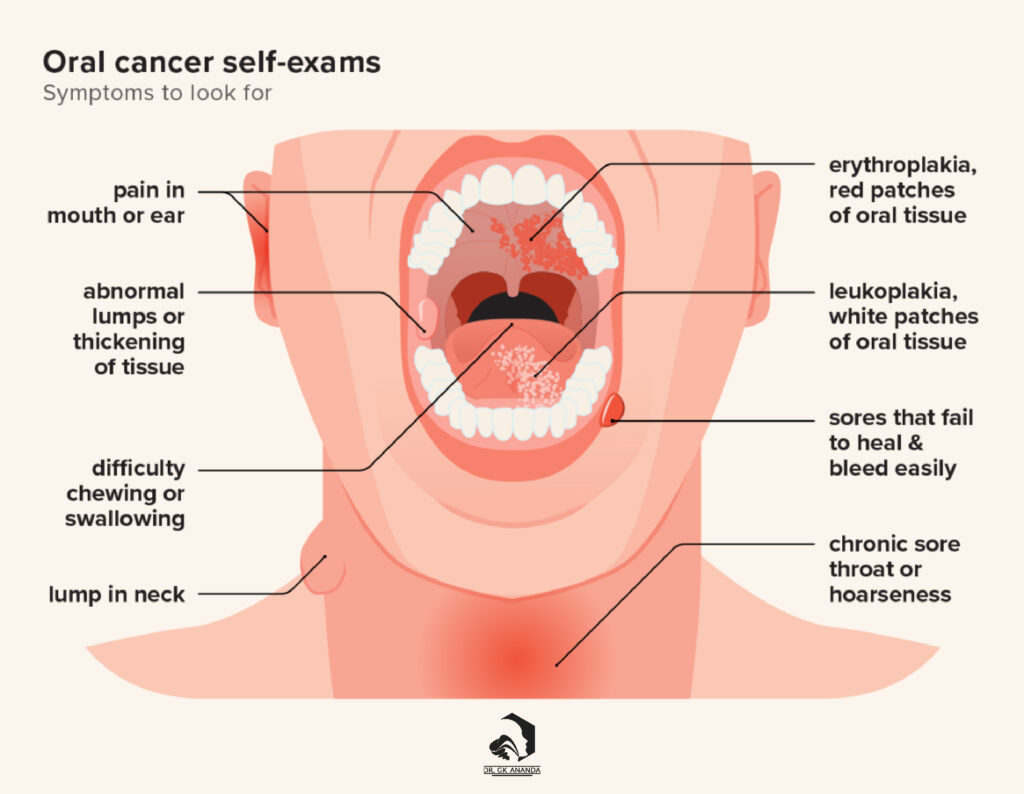
Oral Cancer Signs And Symptoms
The following signs or symptoms may indicate the presence of oral cavity (mouth) and oropharyngeal (throat) cancers:
1. Failure of a lip or mouth sore to heal
2. Persistent sore throat lasting beyond a few days
3. Painful mouth ulcers that do not heal within several weeks
4. Identification of a white or reddish patch on the inner lining of the mouth or tongue, which could be an early indication of cancer and should be examined
5. Unexplained looseness of teeth or failure of tooth sockets to heal after extractions
6. Toothache or discomfort around the teeth
7. Poor fit or discomfort experienced with dentures
8. Presence of a growth or lump in the mouth or throat
9. Persistent, unexplained lumps in the mouth or neck
10. Chronic sore throat or sensation of an obstruction in the throat that persists
11. Mouth pain
12. Ear pain that does not subside within a few days
13. Difficulty or pain while swallowing
14. Difficulty in jaw movement or chewing
15. Trouble moving the tongue
16. Unexplained, long-lasting numbness or abnormal sensation in the tongue, lip, or other areas of the mouth
17. Lump or thickening of the lip
18. Changes in speech, such as a noticeable lisp
19. Unexplained weight loss
20. Persistent bad breath
21. Unusual bleeding in the mouth
22. Alterations in voice
Many of these signs and symptoms can also be attributed to conditions other than cancer, including different types of cancer. If these symptoms do not improve within two weeks, especially if you smoke or consume alcohol, it is advisable to consult a doctor or dentist.
Oral Cancer Causes
The exact causes of each case of oral cavity or oropharyngeal cancer are not fully understood by doctors and scientists. However, they have identified several risk factors and understand how some of them can contribute to the development of cancerous cells.
Cancer can arise from DNA mutations, which involve changes in genes that either activate oncogenes or deactivate tumor suppressor genes. These genetic alterations result in uncontrolled cell growth. The development of oral cavity and oropharyngeal cancer typically requires changes in multiple genes.
Certain genes play a role in regulating cell growth, division, and programmed cell death:
- Proto-oncogenes are genes that normally facilitate cell growth, division, and survival. When a proto-oncogene undergoes a mutation, it becomes abnormal and is referred to as an oncogene.
- Tumor suppressor genes are responsible for maintaining control over cell growth or promoting cell death at the appropriate time.
Scientists speculate that some risk factors, such as tobacco or heavy alcohol use, can damage the DNA of cells lining the mouth and throat, leading to these cancers.
When cells in the mouth and throat are damaged by tobacco and alcohol, the affected layer of cells experiences increased division and replication. This heightened activity raises the chances of DNA copying errors, potentially increasing the likelihood of developing cancer.
Various chemicals present in tobacco have the ability to directly damage DNA. While it remains uncertain whether alcohol directly damages DNA, research has shown that alcohol facilitates the entry of many DNA-damaging chemicals into cells. This may explain why the combination of tobacco and alcohol causes more DNA damage than tobacco alone. Acetaldehyde, a byproduct of alcohol metabolism, is found in saliva. It has been observed to impede normal DNA repair mechanisms and disrupt other DNA-related functions. As alcohol consumption increases, the level of acetaldehyde rises, which may be one way in which alcohol damages the cells lining the oral cavity.
This damage can impair the functioning of specific genes responsible for regulating cell growth initiation or inhibition. Consequently, abnormal cells can begin to proliferate uncontrollably, leading to the formation of a tumor.
How Mouth Cancer Spreads
Metastasis is the term used to describe the spread of cancer cells from the mouth to other areas of the body.
There are two primary ways in which mouth cancer can spread:
- Direct spread: Cancer cells can spread directly to nearby tissues, such as the surrounding skin or the back of the jaw.
- Lymphatic system dissemination: Cancer cells can also spread through the lymphatic system, which consists of a network of vessels and glands throughout the body. These lymphatic vessels produce specialized cells that support the immune system’s infection-fighting capabilities.
When mouth cancer spreads to other parts of the body, it is referred to as metastatic oral cancer or secondaries. Typically, the first site where mouth cancer forms metastases is the lymph nodes in the neck.
If oral cancer metastasizes, it can affect the following areas:
- Other regions within the mouth
- Muscles surrounding the mouth
- Lymph nodes in the neck (referred to as cervical lymph nodes)
- Bone surrounding the mouth, such as the upper or lower jawbone
- Facial skin
- Salivary glands
- Liver
- Lungs
- Distant bones, such as the base of the skull or the spine
- Brain

Oral Cancer Treatment
When diagnosed with oral cancer, a personalized treatment plan will be developed by your healthcare team, taking into account your individual health and detailed information about the cancer. In determining the appropriate treatments for oral cancer, the healthcare team will consider the following factors:
- Size of the cancer: The extent or size of the cancerous growth will be evaluated to determine the most suitable treatment approach.
- Stage of the cancer: The stage of the cancer, which indicates the extent of its spread, will be considered. This helps guide treatment decisions and prognosis.
- Location of the cancer: The specific site where the cancer is located within the oral cavity will be taken into account, as treatment options may vary based on the affected area.
- Overall health and recovery capacity: Your general health and ability to recover from surgical procedures, radiation therapy, or chemotherapy will be assessed to ensure that the chosen treatment is appropriate and well-tolerated.
- Impact on appearance and function: The potential effects of each treatment modality on your appearance and important functions, such as speech, swallowing, and chewing, will be considered. Preserving these functions and maintaining quality of life will be taken into account during treatment planning.
- Personal preferences: Your personal preferences and values will be respected and considered when discussing and determining the most suitable treatment options. Open communication with your healthcare team is essential to ensure your preferences are taken into account.
By considering these factors, your healthcare team will develop a tailored treatment plan that aligns with your specific needs and aims to provide the most effective and personalized care for your oral cancer.
Primary treatment modalities available for individuals diagnosed with oral cavity and oropharyngeal cancers include:
- Surgery: This involves the surgical removal of the cancerous tumor and nearby affected tissues. Surgery may vary depending on the cancer’s size, stage, and location.
- Radiation Therapy: The use of high-energy radiation beams to target and destroy cancer cells. It can be administered externally (external beam radiation) or internally (brachytherapy) based on the specific needs of the patient.
- Chemotherapy: The use of drugs to kill cancer cells or inhibit their growth. Chemotherapy is often used in combination with other treatments, such as surgery or radiation therapy, and can be administered orally or intravenously.
- Targeted Therapy: This type of treatment utilizes drugs that specifically target certain molecules or genes involved in cancer growth. Targeted therapy aims to disrupt specific pathways in cancer cells while minimizing damage to healthy cells.
- Immunotherapy: This approach harnesses the body’s immune system to recognize and destroy cancer cells. Immunotherapy can be administered in various forms, such as immune checkpoint inhibitors or adoptive cell transfer, and is designed to enhance the immune response against cancer.
- Palliative care: This form of care focuses on providing relief from symptoms, pain, and stress caused by cancer, rather than aiming for a cure. Palliative care aims to improve the quality of life for individuals with advanced oral cavity and oropharyngeal cancers.
These treatment options may be used individually or in combination, depending on the specific characteristics of the cancer and the patient’s overall health. The choice of treatment will be determined through a comprehensive evaluation by the healthcare team, considering factors such as the stage, size, and location of the cancer, as well as the patient’s preferences and overall well-being.
A comprehensive healthcare team specializing in the treatment of oral cancer may include the following professionals:
- Head and neck surgeon (also known as an otolaryngologist or ENT doctor): Specializes in surgical procedures related to the mouth, jaw, face, and neck.
- Head and neck reconstructive surgeon: Specializes in reconstructive surgeries involving the head, neck, and facial areas, including plastic surgery.
- Oral and maxillofacial surgeon: Specializes in surgical interventions related to the mouth, jaw, and face.
- Medical oncologist: Specializes in the treatment of cancer using drug therapies.
- Radiation oncologist: Specializes in delivering radiation therapy to treat cancer.
- Maxillofacial prosthodontist: Specializes in the replacement of lost tissues, teeth, and prosthetics related to the head, neck, and mouth.
- Dentist: Provides dental care and may perform necessary dental work before initiating treatment.
- Speech therapist (speech-language pathologist): Assesses and helps manage speech difficulties that may arise due to oral cancer or its treatment.
- Registered dietitian: Conducts nutritional assessments and provides guidance to address any nutrition-related issues caused by oral cancer.
- Social worker: Offers support and assistance in managing the emotional and practical aspects of coping with oral cancer.
Before beginning treatment, a nutritional assessment may be conducted by a dietitian to evaluate the impact of oral cancer on your nutrition. In cases where adequate nutrition is compromised, a feeding tube may be recommended to ensure sufficient nutrition and weight maintenance during treatment.
Speech therapists play a crucial role in evaluating and managing speech problems that may arise as a result of oral cancer or its treatment.
It is also important to undergo a comprehensive dental examination before initiating treatment, as dental work may be necessary.
If you are a smoker, your healthcare team will provide guidance and support to help you quit smoking, as smoking can reduce the effectiveness of cancer treatment.
Treatment for oral cancer typically starts with surgery, followed by radiation therapy, sometimes combined with chemotherapy. Reconstruction may be required to restore structures in the mouth and jaw, as well as to address speech and swallowing difficulties. Reconstruction plans are developed alongside the overall treatment plan, and it is essential for the healthcare team involved in reconstruction to assess your expectations before initiating any surgical or other treatment interventions.